Conditions
Cervical Stenosis and Cervical Myelopathy
Cervical Spine Anatomy
Cervical stenosis and myelopathy is closely related to the anatomy of cervical spine. The cervical spine is composed of seven vertebrae, the discs and ligamentous bands between these bands, but there are eight cervical spinal nerve roots. In terms of bony anatomy, the cervical vertebra is composed of a vertebral body (only C1 vertebra does not have a body, instead it has an anterior arch) connected to a posterior neural arch that together enclose the spinal canal, which includes the spinal cord.
The spinal cord and spinal nerve roots carries signals from the brain into our arms, legs and body and, at the same time, carries signals back. These signals control muscles and are responsible for feeling in certain parts of the arm, leg or body.
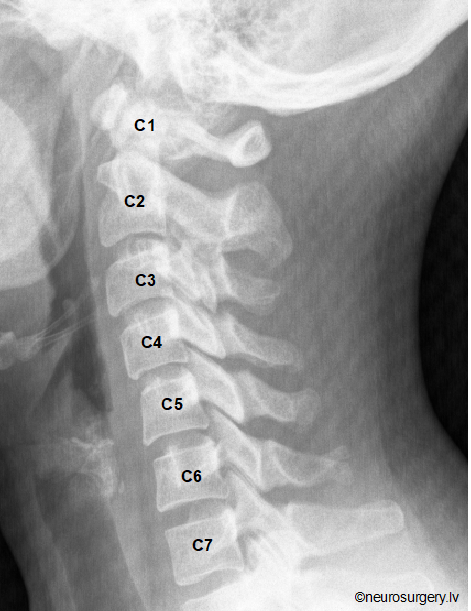
Image: X-Ray of neck, showing cervical vertebrae alignment
Cervical Myelopathy / Cervical Spondylotic Myelopathy
Cervical myelopathy is a condition describing damage of the spinal cord due to severe narrowing (stenosis) of the cervical spinal canal. Classically, it has an insidious onset progressing in a stepwise manner with functional decline. Without treatment, patients may progress toward significant paralysis and loss of function.
Certain patients are more predisposed to myelopathy due to a congenitally narrowed cervical spinal canal. Subsequent progression of stenosis or a cervical disc herniation will then more likely results in myelopathy at this level.
Cervical spondylotic myelopathy will develop in approximately 100% of patients with grater than 60% canal stenosis.
Other causes of cervical myelopathy may include:
– Rheumatoid arthritis of the neck, ankylosing spondylitis
– Spinal tumors and cancers
– Spinal infections
– Whiplash injury or other cervical spine trauma.
What are the symptoms of cervical stenosis and myelopathy?
- Hand clumsiness and a limited ability to perform fine motor tasks such a buttoning a shirt, combing hair, holding small objects; handwriting may become worse.
• Unsteadiness, requiring holding onto objects more frequently while walking. Gait may become noticeably wobbly.
• Weakness in arms and/or legs.
• Neck pain and stiffness, reduced range of motion.
• Changes in bowel or bladder control.
• Cervical radiculopathy (nerve root compression or pinched nerve). It will manifest as pain traveling from the neck into a specific region of either shoulder, arm, forearm or hand. This may be accompanied by numbness in a similar distribution or weakness in specific muscles. Radiculopathy will develop secondary to irritation and/or compression of a spinal nerve root in the neck.
In case there is a need for our specialist opinion, we are happy to help. We provide appointments and consultations for both – residents of Latvia and patients from abroad, including remote appointments via video-call. There are a number of ways to schedule appointment with one of our specialists – electronically (for Latvian residents) or requesting a remote appointment via video call by email or through the telephone contact.
How is cervical stenosis and myelopathy being diagnosed?
- If you have worsening function, pain, numbness or weakness in one or both of your arms and/or legs that is not relieved following a short period of observation and taking over-the-counter (OTC) painkillers, you should certainly see a doctor.
- History of how your symptoms began and how they progressed is very important.
- Physical examination of neck and nerve function in your arms and legs as well as checking your balance and testing your gait is important to figure out the cause of the problem.
- X-ray may be requested and in many patients it will show signs of degenerative changes. Bending x-rays (flexion-extension x-rays) of the neck may show a degree of “slip slide” and may discover instability between the neck vertebrae.
- Magnetic resolution imaging (MRI) of the neck pictures allow to visualize structures that may be impinging on the spinal cord and/or the nerve roots. MRI is the best scan to evaluate spinal cord, nerve roots and disc space. Canal space of less than 10mm indicates stenosis.
- Computerized tomography (CT) scans after injection of dye into the spinal canal (CT myelogram) may be required in some patients who cannot undergo MRI, e. g., those with pacemakers or cochlear implants or for those in whom MRI provides limited information, e. g., patients with extensive metal in the spine.
- Electromyogram (EMG) and nerve conduction studies in some patients may help distinguish cervical radiculopathy from other nerve problems in the arm, forearm and hand such as carpal tunnel syndrome, cubital tunnel syndrome etc.

Image: MRI of neck, showing degenerative changes and severe spinal cord compression at C4/C5 (green arrows) and myelopathic changes in the spinal cord at/ below the level of compression (red asterisk).
What treatments are available for cervical stenosis and myelopathy?
Non-surgical care
Up to 19% of asymptomatic patients have major cervical abnormalities on MRI. In patients with mild cervical stenosis and without clinically obvious myelopathy, cautious non-surgical (conservative) care is an option. This generally begins with patient education regarding their condition and disease. Patients need to understand that narrowed cervical spinal canal can predispose them to myelopathy at some point in the future.
Prolonged bed rest can lead to deconditioning and is generally not recommended. Non-surgical management should include OTC anti-inflammatories, corticosteroid injections, physical therapy, cervical collar brace, modification of activities. Physical therapy is an important part of their treatment process. However, in patients with severe spinal canal stenosis and symptomatic myelopathy these short-term alternatives will not be a definitive treatment.
Surgery
In the setting of unsuccessful non-surgical care or progression, surgical management should be highly considered. The goal of surgery is to increase the canal space which will lessen/ eliminate the cord compression.
Surgery is either anterior (through the front) or posterior (from the back) decompression of the tight area of the spinal canal. Several factors will be considered in choosing the type of surgery. These will include the exact location of any compression on spinal cord or nerve roots, the number of levels at which there is compression and the overall alignment of particular cervical spine and patient’s overall medical condition.
Posterior decompression
Many patients may benefit from posterior decompression (laminoplasty, laminectomy or laminotomy), when surgery is carried through the back of the neck. Tailored to particular problem incision is made directly over the previously fluoroscopically (x-ray) marked area. In laminoplasty (open door laminoplasty), a hinge is created with high-speed drill on one side of the back of the vertebra and the lamina lifted up on this hinge to make room for the spinal cord, and small titanium plates and screws are used to fix the laminae in the open position. In laminectomy, the back of the vertebra (lamina) is completely removed.
Anterior decompression
When surgery is carried out through the front of the neck, a small horizontal incision is made in the front of neck. Intraoperative fluoroscopy (x-ray) imaging before skin incision and during surgery is essential to avoid level errors. Under operating microscope, anterior decompression, removing of herniated discs, bone spurs and ossified ligaments, is performed. A fusion surgery is done at the same time as the anterior cervical decompression in order to stabilize the cervical segment. A fusion involves placing implants where the disc and/or vertebra originally was in order to provide stability and strength to the area.
We provide world class neurosurgical treatment for Latvian residents and for international patients. Learn more here if you are international patient considering having treatment with us.
The venue for surgical interventions is perfectly equipped and comfortable private hospital in Riga – “Aiwa clinic”.
Prognosis
A consensus statement is recommending surgical intervention once a diagnosis of cervical myelopathy has been made. Timeless of intervention is critical. Patients with milder myelopathy and less then six months of symptoms have improved outcomes after surgery.
Surgery can immediately eliminate spinal cord compression. Therefore, the spinal cord function can rapidly improve during the first week after surgery. A high rate of recovery is observed within six months after surgery. After six months, recovery continuously is improving in the young and middle-aged patients and declining in older patients. According to recent study, in all three age groups recovery rates were 41, 53, 63, 64 and 64% at 1 week, 1 month, 6 months, 1 year and final follow-up, respectively.
A poor prognosis is associated with age, involved cervical levels, symptomatic duration of more than 18 months, increased cervical spine range motion, associated trauma, and female gender.
Complications associated with cervical stenosis surgery are not frequent, significantly different and are not severe in all age groups.
Surgical treatment has become the main method of treatment for cervical spondylotic myelopathy. Although elderly patients with cervical myelopathy have more prolonged symptoms, greater number of involved levels and more severe damage of the spinal cord than the younger patients, they can still attain the similar surgical effects as those young patients when the surgical approach is appropriate, and the decompression is complete.
What does surgery mean to me as a patient?
By deploying a minimally invasive and microsurgical techniques, cervical spine decompression surgery is patient friendly and easy to tolerate.The smaller the surgical trauma, at any age considered, but especially in the elderly, the significantly faster the recovery and return to daily activities will be. This is especially true for the elderly, where results of minimally invasive surgery are significantly better. Patients only need to spend one night at the hospital after the operation, after that the patient is released to go home. Cervical collar may be used for comfort up to few weeks after surgery.
In case you are considering having a Surgery with us, please check page for International patients.