Conditions
Spinal Fractures
Introduction to Traumatic Spinal Injuries
Spinal trauma and fractures are much more serious than a broken arm or leg. If a vertebra fractures or shifts out of place due to trauma, bone fragments can compress the spinal cord or nerve roots, causing severe damage with potentially devastating consequences.
Most spinal fractures occur due to falls, intense sports activities, or motor vehicle accidents. The severity of an injury can vary, ranging from minor ligament and muscle strains to severe vertebral fractures, dislocations, or even spinal cord damage resulting in paralysis. Depending on the severity, you may experience pain, discomfort, difficulty moving your arms or legs, or an inability to walk. While many minor fractures can be treated conservatively (without surgery), severe fractures may require surgery to restore spinal anatomy.
Spinal Anatomy
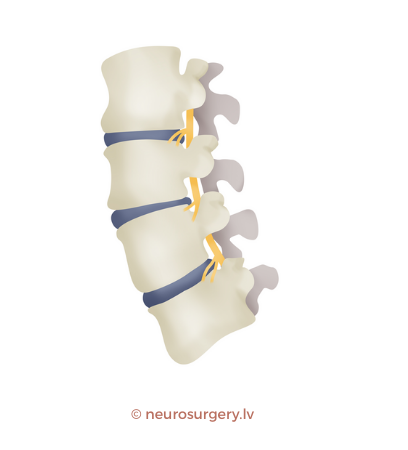
Understanding spinal anatomy helps clarify spinal fractures and traumatic injuries. Your spine is the body’s main structural support, allowing you to stand upright, bend, and rotate.
The human spine consists of 33 vertebrae, supported by intervertebral discs, ligaments, and muscles. The spine is divided into:
- Cervical spine (7 vertebrae)
- Thoracic spine (12 vertebrae)
- Lumbar spine (5 vertebrae)
- Sacral spine (3–5 fused vertebrae forming the sacrum)
The spinal canal is a tunnel within each vertebra, housing the spinal cord and nerve roots. The spinal cord starts at the base of the skull and ends between the first and second lumbar vertebrae. Below this level, the spinal canal contains a bundle of nerves known as the cauda equina (Latin for "horse’s tail," due to its resemblance on MRI scans), which extends down to the lower sacrum.
Your spinal cord functions like a high-speed highway, transmitting huge amounts of information between the brain and the rest of the body. Nerve roots branch off the spinal cord at each vertebral level, passing through intervertebral openings and continuing as nerves and nerve plexuses.
An injury at any part of the spine can be serious, especially if a vertebra is fractured or dislocated, the fracture is unstable, or if the spinal-supporting ligaments are torn.
Causes of Spinal Fractures
1. Osteoporosis
Osteoporosis is the leading cause of spinal fractures, primarily affecting older adults. Even minor household accidents (e.g., falls or small mishaps at home) can lead to vertebral compression fractures, reducing vertebral height and causing deformities.
While both men and women can experience osteoporotic fractures, women are at higher risk. One in four women with vertebral fractures remains undiagnosed.
If a doctor diagnoses an osteoporotic compression fracture, the risk of new fractures increases fivefold. If two fractures have already occurred, the risk increases twelvefold (!).
Factors increasing the likelihood of osteoporosis include:
- Female gender
- Diagnosed osteoporosis or osteopenia
- Age over 50
- Previous vertebral fractures
- Smoking
- Vitamin D deficiency
- Long-term corticosteroid use
Other causes that weaken bones and lead to compression fractures include radiation therapy, cancer, chemotherapy, infections, long-term steroid use, and hyperthyroidism (excess thyroid hormone production, which can also lead to weight loss, hand tremors, and irregular heartbeat). Additionally, low estrogen levels, smoking, alcoholism, anorexia, kidney disease, and certain medications (such as proton pump inhibitors, which reduce stomach acid) can decrease bone density, leading to osteoporosis as a final outcome.
2. Traumatic Injuries
Spinal trauma is the second most common cause of spinal fractures. Traumatic fractures can occur in any part of the spine, including the cervical, thoracic, lumbar, sacral, and coccygeal regions. However, 50% of fractures occur at the thoracolumbar junction.
Approximately 40 spinal injuries per year occur per million people, with 80% of patients being men, averaging 30 years of age.
The leading causes of spinal injuries are:
- Motor vehicle accidents (48%)
- Falls (16%)
- Assaults (12%)
- Sports injuries (10%)
- Work-related accidents
Types of Spinal Fractures
Spinal fractures come in various forms, including:
- Compression fractures
- Burst fractures
- Flexion-distraction (Chance) fractures
- Dislocated fractures (with bone fragment displacement)
Doctors may describe fractures using terms like stable, unstable, minor, or significant, which help clarify the severity of the injury.
Compression Fractures
Patients with osteoporosis or bone diseases (e.g., cancer) are prone to this type of fracture. Vertebrae can withstand a certain level of pressure, but when a weakened vertebra undergoes excessive stress, it may collapse. A wedge fracture is a subtype, occurring when the front part of the vertebra compresses into a wedge shape, causing spinal deformity.
Burst Fractures
Burst fractures typically result from high-impact trauma, such as car accidents or falls from significant heights. A strong vertical force can shatter the vertebra into multiple pieces, compressing the spinal canal and potentially damaging the spinal cord or nerves. Burst fractures are more severe than compression fractures.
Flexion-Distraction (Chance) Fractures
These fractures often occur in car accidents, when the body is forcefully thrown forward, sometimes referred to as a seatbelt injury. While the spine is designed to flex forward, high-speed and high-intensity movement can exert excessive stress, leading to vertebral fractures.
Dislocated Fractures
Dislocated fractures happen when vertebrae shift significantly. Such fractures often affect all three spinal columns, making the spine unstable and increasing the risk of spinal cord or nerve damage.
Stable vs. Unstable Fractures
- Stable fractures do not cause spinal deformities or nerve damage and allow the spine to maintain sufficient structural support.
- Unstable fractures pose greater risks, potentially leading to severe spinal cord or nerve injuries, resulting in mobility impairment or even paralysis.
Even if no immediate neurological symptoms (like movement loss, sensory deficits, or bladder/bowel dysfunction) are present, unstable fractures can deteriorate, causing progressive spinal damage.
Severity of Spinal Cord Injuries
- Complete spinal cord injury results in a total loss of movement and sensation below the injury level.
- Incomplete spinal cord injury causes partial impairment, where some function remains intact.
Minor vs. Major Fractures
- Minor fractures involve small parts of the vertebra, such as intervertebral joints or transverse/spinous processes. These fractures do not significantly affect spinal stability.
- Major fractures affect the vertebral body or arches, compromising spinal integrity and increasing the risk of instability and nerve damage.
Symptoms of Spinal Fractures – When to Seek Medical Help
Seek immediate medical attention if you experience any of the following after trauma:
- Severe pain or discomfort in the spine or skull
- Tingling in the fingers or toes
- Difficulty walking or moving limbs
- Bladder or bowel dysfunction
- Band-like discomfort in the chest (pain, pressure)
- Breathing problems following trauma
- Swelling or bruising on the head or spine
Diagnosis of Spinal Fractures
At the emergency department, an urgent care doctor will perform an initial neurological and general examination. Depending on the mechanism and severity of the trauma, further diagnostic imaging will be conducted. Specialists may be called in for detailed evaluation and management.
Radiography
Radiography uses X-rays to create images that allow the visualization of bones and vertebrae, enabling the assessment of fractures and dislocations. Spinal X-rays can be taken separately for three main spinal regions:
- Cervical spine
- Thoracic spine
- Lumbar spine
In some cases, imaging is performed for specific vertebrae (e.g., C1 and C2 in the cervical spine). Overall, spinal X-rays are considered a safe method, as the radiation dose used is minimal, resulting in low risks. However, young children and pregnant women are more sensitive to X-rays, making the examination potentially more harmful for them.
CT/DT (Computed Tomography) Examination
Computed tomography (CT) or digital tomography (DT) uses X-ray radiation, which is processed by a computer to generate detailed spinal images. CT is a relatively safe, non-invasive method, producing three-dimensional images of the spine, making it more precise than standard X-rays. It enables the evaluation of bones and, to some extent, soft tissues.
MRI Examination
For a detailed assessment of the spine and related injuries, a doctor may recommend a magnetic resonance imaging (MRI) examination. Unlike X-ray and CT scans, MRI uses magnetic fields instead of radiation, making it a safer alternative without harmful ionizing radiation.
MRI is particularly effective at visualizing soft tissues—including the spinal cord, nerves, and surrounding tissues. However, it may not be as precise as CT scans for assessing vertebrae and fracture lines.
Importantly, MRI can detect bone edema (swelling). In cases of osteoporotic fractures, where vertebral height reduction is minimal, a fracture may not be clearly visible on X-rays or CT scans. MRI can help identify bone edema, confirming whether the fracture is recent (acute) or old.
How Are Spinal Fractures Treated?
The treatment of a spinal fracture depends on several factors:
- What caused the fracture?
- What type of fracture is it? (Stable/Unstable)
- Which vertebra is affected, and at what location?
Conservative (Non-Surgical) Treatment
Most spinal fractures do not require surgery. The most common treatment methods include:
Spinal Orthoses (Braces)
To stabilize the spine and promote healing of an injured thoracic and/or lumbar vertebra, a special spinal brace (orthosis or corset) may be required for immobilization. Typically, these must be worn for several months. Your doctor will discuss the type of brace needed and its duration of use.
Common spinal brace types include:
- Thoracolumbar orthoses (TLSO) – used for thoracic fractures, with less rigid versions for elderly patients.
- High lumbar orthoses – used for thoracolumbar transition fractures.
- Standard lumbar orthoses – used for lumbar fractures.
In cases of cervical spine fractures, if stable, treatment typically involves rigid or semi-rigid neck braces. For unstable cervical spine fractures, stabilizing surgery is performed first, followed by brace immobilization. Halo vests are occasionally used for upper cervical fractures requiring extended immobilization.
Pain Management
Pain relief is crucial, especially in the first few weeks after trauma. Generally, over-the-counter pain medications, such as acetaminophen (Paracetamol, Tylenol), ibuprofen (Ibumetin, Ibustar), or naproxen (Nalgedol), are sufficient to manage fracture-related discomfort.
Physical Therapy
Physical therapy helps increase overall strength, prevent bone mass loss, and reduce future spinal fracture risk. Typically, therapeutic exercises are performed at home or with a physiotherapist.
Osteoporosis Treatment
If osteoporosis is diagnosed, a doctor may recommend medications to strengthen bones and reduce fracture risk. Additionally, calcium, magnesium, and vitamin D3 supplements are advised to support bone metabolism and healing.
Surgical Treatment for Spinal Fractures
Common surgical treatment options include:
- Vertebroplasty
- Kyphoplasty
- Spinal fixation with metallic implants
Vertebroplasty
A minimally invasive procedure, vertebroplasty involves inserting a needle into the fractured vertebra (vertebroplasty needle) without making surgical incisions. The surgeon injects a specialized bone cement through the needle to strengthen and stabilize the fracture.
Since the cement hardens within about 30 minutes, patients can usually go home within a few hours, and fracture-related pain disappears almost immediately.
Kyphoplasty
Similar to vertebroplasty, kyphoplasty involves inserting a special balloon into the fractured vertebra before injecting bone cement. The balloon creates space for cement injection and sometimes restores lost vertebral height. This method reduces the risk of cement leakage.
Both vertebroplasty and kyphoplasty are preferred for stable vertebral fractures.
Spinal Fixation with Metal Implants
Spinal fixation with metal implants is the primary surgery for unstable fractures. Following surgery, patients must remain hospitalized for a period, and recovery time is longer, particularly if a spinal cord injury is present.
Fixation uses implants such as rods, plates, and screws to promote fracture healing and spinal stability. These function as internal supports. Modern implants are MRI-safe, meaning they do not interfere with MRI scans. Materials commonly used include stainless steel, titanium, cobalt-chromium, nickel, tantalum, or non-metallic substances.
After spinal fixation, a brace is worn for about three months for additional stabilization. Brace selection depends on the fracture location:
- Thoracic fractures → TLSO braces
- Thoracolumbar transition fractures → TLSO or high lumbar braces
- Lumbar fractures → Standard lumbar braces
Your doctor or surgeon will recommend appropriate treatment based on your health condition and fracture type. Treatment strategies may vary depending on the fracture mechanism and overall health. If a tumor caused the fracture, surgical strategies may involve tumor removal before spinal stabilization.
Consequences of Untreated Spinal Fractures
- Chronic pain
- Posture problems
- Reduced activity and social isolation
- Lower quality of life
- Decreased self-confidence
- Higher risk of future fractures
- Nearly double the mortality rate compared to healthy individuals